In today’s complex U.S. healthcare market, healthcare facilities regularly seek new ways to serve patients’ needs, meet insurers’ criteria, and follow legal requirements. The rise of primary care clinics, urgent care facilities, and hospital-owned satellite emergency facilities are noticeable and useful additions in communities around the country. They often offer cost savings, quicker service, and, in some cases, the only care in areas without immediate access to hospitals. Recently, a new twist has been added to the mix of “pop-up” medical facilities. Many medical care providers view these new facilities as “disruptors.” For patients, these new facilities can be confusing and, worse, can result in enormous bills. What are these new facilities called? Independent, non-hospital affiliated freestanding emergency rooms (FSERs).
After taking a close look as FSERs and assessing a few cases directly (two cases are described later in this article), SphereMD has some well-founded, fact-based reservations about independent freestanding ERs. SphereMD is sharing its research and findings so ship owners and crew members can avoid costly surprises later.
Rise of Independent Freestanding ERs
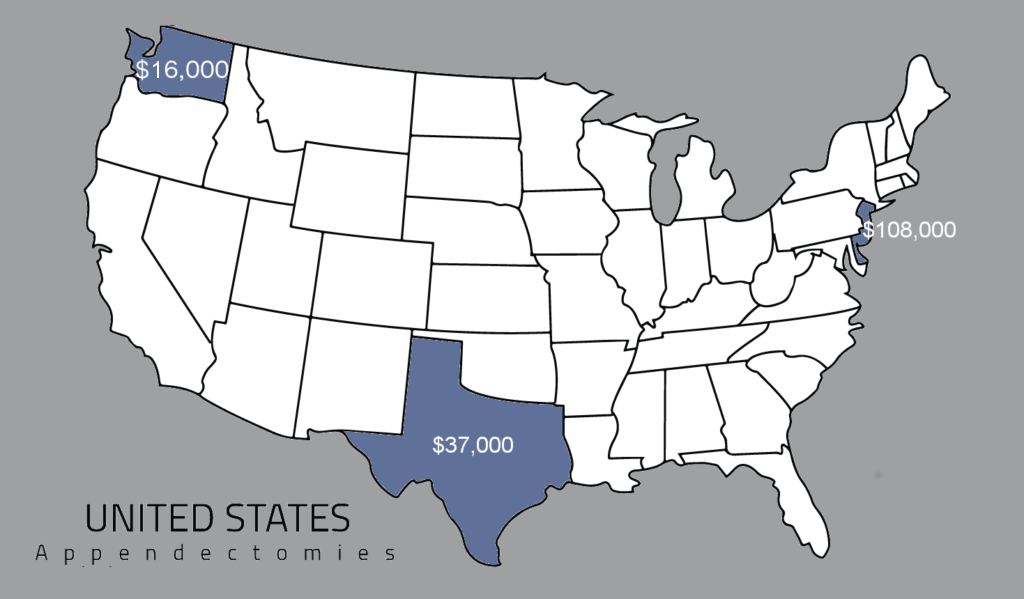
At the basic level, independent freestanding ERs are stand-alone facilities where people can receive emergency healthcare any time of day, in a nearby facility. FSERs were initially conceived as a way to offer emergency room services and emergency care access in areas where hospitals were nonexistent or miles away, such as in rural or low-income areas. Sadly, the facilities have not yet been deployed that way. Instead, they are most likely to be found in affluent areas where profits are more readily available, including Texas and other Gulf states.
FSERs began making a strong presence in healthcare in Texas after a 2009 law allowed the establishment of non-hospital affiliated emergency rooms. Since then, independent freestanding ERs have spread across Texas and through other states. In fact, according to a recent Washington Post article, in 2017, “across 32 states, more than 400 freestanding ERs provide quick and easy access to care.”
Increased access to healthcare without having to go to the hospital sounds like a positive development for mariners, but the Washington Post article goes on, the freestanding ERs “also are prompting complaints from a growing number of people who feel burned by hospital-size bills, like $6,856 for a cut that didn’t require a stitch or $4,025 for an antibiotic for a sinus infection.”
Over $6,000 to treat a cut? That’s not a typo. While the convenience of freestanding ERs is appealing, their costs are stirring up serious controversy.
The Controversy
To be fair, on the upside, the main draw of independent freestanding ERs is convenience. To patients, they look like the more-affordable urgent care centers but with the added benefit of offering limited emergency services. These facilities can even transfer critical patients to hospitals when needed. The urgent care appearance is misleading, though. As the Texas Association of Health Plans explains:
Though freestanding ERs tend to have the same look and feel of urgent care centers, many consumers are unaware that, unlike urgent care centers, these facilities are often out of network and can charge patients up to 10 times more for the same services.”
-TAHP (http://tahp.org/advocacy/freestanding-ers)
Keep in mind, freestanding ERs are still emergency rooms, which means they charge emergency room prices. In addition, many independent freestanding ERs also charge a facility fee. Therefore, sending crew members to an independent freestanding emergency room is just like paying an extra fee to receive emergency room treatment. As most shipowners and crew members know, emergency rooms are already the most expensive and least efficient venues for non-emergency healthcare. Adding an extra fee on top of ER prices further compounds the problem.
In side by side comparisons, independent freestanding ERs are dramatically more expensive than typical urgent care facilities and medical clinics. For example, as mentioned, freestanding ERs charge higher base fees and usually present two separate bills—one for the facility and one for the emergency services. In non-emergency clinics, patients receive one bill for a medical service, without the added “facility fee” bill. In addition, like hospital emergency rooms, freestanding ERs tend to overuse services, which increases costs. In all emergency rooms, patients are more likely to receive more tests and services than they would in an urgent or primary care clinic.
To better understand the differences, SphereMD documented two real-life cases handled by independent freestanding ERs.
Case 1
Injury: Small puncture wound to the foot; no fractures or breaks.
Treatment: Bandage, no other treatment rendered
Independent Emergency Room Provider
Cost: $4,173.02
Cost Breakdown:
- Physician Examination – $667.01
- Pharmacy General – $257.25
- Medical Supplies – $92.35
- X-Ray Left Foot – $707.16
- X-Ray Right Foot – $707.16
- Emergency Room General – $1,721.40
- Discharge Medication (Ciprofloxacin 500mg qty. 14) – $20.69
Estimated Urgent Care Facility
Cost: $220.69 – $645.69*
Cost Breakdown:
- Examination – $125–$300
- Pharmacy – $75
- Medical supplies: – 0
- X-Ray Left Foot – $125*
- X-Ray Right Foot – $125*
- Emergency Room General – 0 (included in the examination fee)
- Discharge Medication (Ciprofloxacin 500mg qty. 14) – $20.69
Savings: Over $3,525

*Note: X-rays may not have been ordered in an urgent care facility as this decision would have been based on clinical discretion vs. protocol. Eliminating the x-rays would save an additional $250.
SphereMD asked the freestanding ER about the x-rays in this case. The ER responded that the x-rays are protocol for puncture wound cases. This approach is both medically aggressive and expensive. Treatments based on protocol vs. clinical judgement brings into question the necessity of much of the care provided. In SphereMD’s opinion, this practice leads to overuse of services. In general, emergency rooms, freestanding and in hospitals, are notorious for overusing services.
In comparison, the same care could have been provided in an urgent care facility or doctor’s office for a fraction of the cost, for a savings of over $3,525, as shown.
Case 2
Injury: Abdominal pain
Final diagnosis: Constipation
Independent Emergency Room Provider
Cost: $3,346.79
Cost Breakdown:
- Initial Exam – $752.40
- EKG – $296.27
- X-Ray Abdomen, one view – $858.00
- CBC – $231.00
- CMP – $615.12
- Troponin – $297.00
Estimated Urgent Care Facility
Cost: $711.50
Cost Breakdown:
- Examination and blood draw – $430
- EKG – $250
- CBC – $31.50
Savings: $2,635.29
Like Case 1, Case 2 demonstrates another overuse of services by an ER. In this case, an urgent care facility most likely would not have ordered several of the lab tests run by the freestanding ER. Further, the blood test costs are outrageous. To compare, the lab SphereMD uses charges the following prices:
- CBC – $31.50
- CMP – $38.25
- Troponin – $132.75
- CK-CM – $137.50
- CK-CM (Cardiac Enzymes) – $297.00
SphereMD’s total lab charges would be $340 vs. $1,440.12 charged by the ER. Remember, many of these tests would not have been ordered by an urgent care facility in the first place.
Based on SphereMD’s experience, if this patient had visited an urgent care facility instead of an independent freestanding ER, the patient would have received an examination with a blood draw, an EKG, a CBC, and no other services, for an estimated savings of $2,635.29, as shown.
As you can see, in both cases, patients were charged outrageous prices given the underlying medical issues. These typical examples are presented to caution shipowners and crews from using independent freestanding ERs, especially for non-emergency issues. This might sound like common sense, but without having this background information, it might not be clear how a medical issue is being handled.
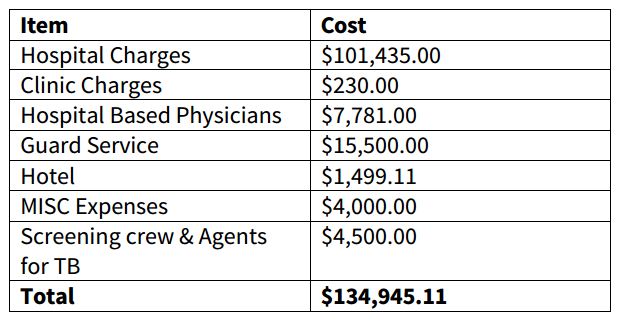
Medical Assignment
A key back-end detail in both cases is that the independent freestanding ER assigned their billing rights to a third party who arranged for the patients to be taken to the FSER in the first place. Most likely, the third-party provider has an arrangement in place that would increase their profits by sending patients to the FSER instead of more appropriate facilities, such as urgent care centers. This arrangement may or may not be transparent to shipowners and crew members.
Vigilance Required
With such a wide variety of facilities available, medical services require vigilance. Facilities need to be vetted and medical issues need to be treated appropriately. In Texas and elsewhere, independent freestanding ERs are being used to treat mariners. SphereMD has reviewed several cases in addition to the two described here in which patients did not require emergency care. Instead, the cases could have been treated in less expensive venues, such as outpatient clinics or urgent care centers. As a medical manager, SphereMD can help shipowners and crews attain the best services at the most affordable prices. SphereMD keeps all records transparent and removes all concerns about patients possibly being directed to independent freestanding ERs or other facilities for kickbacks.
SphereMD Recommendations
To help manage medical situations, SphereMD, a respected and experienced medical management company, has a few recommendations on how to avoid the pitfalls of independent freestanding ERs:
- SphereMD recommends that all shipowners and crew members know about the existence and practices of independent freestanding ERs. This knowledge keeps shipowners one step ahead of high costs.
- SphereMD recommends contacting a P&I Club for even small medical matters in the United States, especially in the Gulf area.
- Finally, to ensure the best medical treatments at the most affordable prices, SphereMD recommends having a medical manager handle both small and large cases, especially in the United States. Leaving medical choices to agents or other non-medically informed entities can result in dramatically higher costs and subpar care.
 Meeting Service Goals in Panama
Meeting Service Goals in Panama Taking Precautions
Taking Precautions

 SphereMD specializes in coordinating, managing, and reviewing medical cases in an ethical, transparent, and cost-effective manner. We yield tangible and significant financial benefits to our clients while ensuring that your crew members receive the highest quality of care possible, every day of the week, 24 hours a day, 365 days a year.
SphereMD specializes in coordinating, managing, and reviewing medical cases in an ethical, transparent, and cost-effective manner. We yield tangible and significant financial benefits to our clients while ensuring that your crew members receive the highest quality of care possible, every day of the week, 24 hours a day, 365 days a year.